Philip Imohi, Michael Egbe, Frank Eyam, Cajetan Obi, Antor Ndep, Olusola Sanwo, Satish Raj Pandey, Hadiza Khamofu, Robert Chiegil, Moses Bateganya, & Ezekiel James
In alignment with the global drive toward the control of the HIV epidemic, members of the FHI 360 team working with the Strengthening Integrated Delivery of HIV/AIDS Services (SIDHAS) project, funded by the U.S. Agency for International Development (USAID), initiated the mapping of potential hot spots in communities using Geographic Information System (GIS). The goal was to further target HIV testing, increase case finding, and achieve treatment saturation across all supported local government areas (LGAs) in Cross River State, Nigeria.
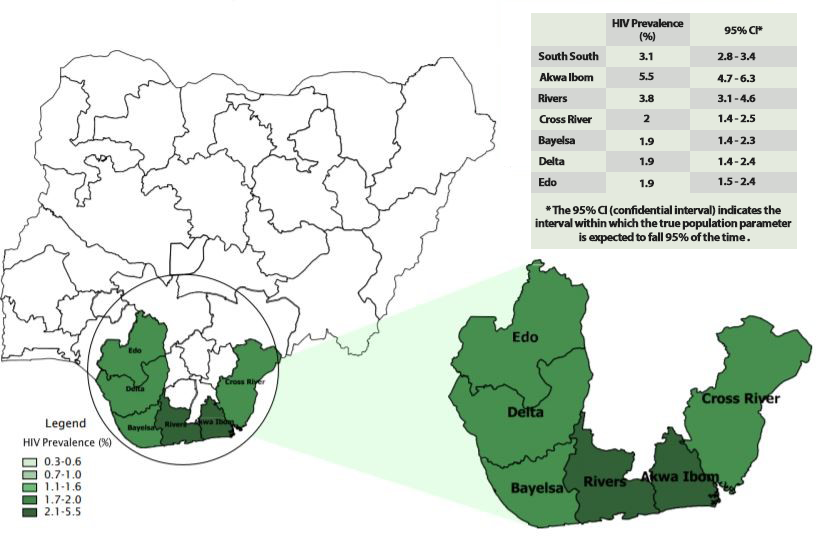
Cross River has an HIV prevalence of 2.0 percent (Figure 1) and high unmet need for antiretroviral therapy (ART) and other HIV services. Most of the adjacent states also have prevalence rates higher than the national average of 1.4 percent; Abia, 2.1 percent; Akwa Ibom, 5.5 percent; Benue, 5.3 percent; and Ebonyi, 0.8 percent. The Revised National HIV and AIDS Strategic Framework 2019–2021 identifies low access to and limited coverage of quality HIV testing services (HTS)—estimated nationally at 37 percent—as limiting factors in fast-tracking the national response toward ending the HIV epidemic in Nigeria.2 Increasing access to high-quality comprehensive HIV prevention, treatment, care, and related services through improved efficiencies in service delivery is the main objective of SIDHAS in Cross River and the surrounding high-burden states.
Figure 1. HIV prevalence by state in the South-South Zone, Nigeria (Source: NACA, 2019)
A key component of the SIDHAS project in Cross River is the use of Community ART Management (CAM) teams—an initiative adopted to extend HIV services from supported health facilities to the community. Sixteen CAM teams were constituted in Cross River and each of these mini-mobile health groups includes a medical doctor, pharmacist, laboratory scientist, partner notification officer, case manager, HIV identification expert, and data entry clerks. These teams conduct community outreach and visit non-SIDHAS supported facilities as potential locations to reach people at risk of HIV with HTS.
To enhance targeted community HTS, the Cross River State SIDHAS team introduced mobile technology and GIS mapping to complement other strategies being used for improved case identification. The first step was the mapping of potential hot spots in the community—locations where PLHIV and individuals at high risk of exposure to HIV were most likely to be found. These sites included patent medicine vendors, private laboratories, healing homes, prayer houses, community pharmacies, traditional birth attendants, and others (Figure 2).
Figure 2. Hot spots in Akpabuyo local government area (LGA), Cross River data (Note: Cold spots and not-significant clusters correspond to areas where HIV positivity is low [on average, less than 30%]).
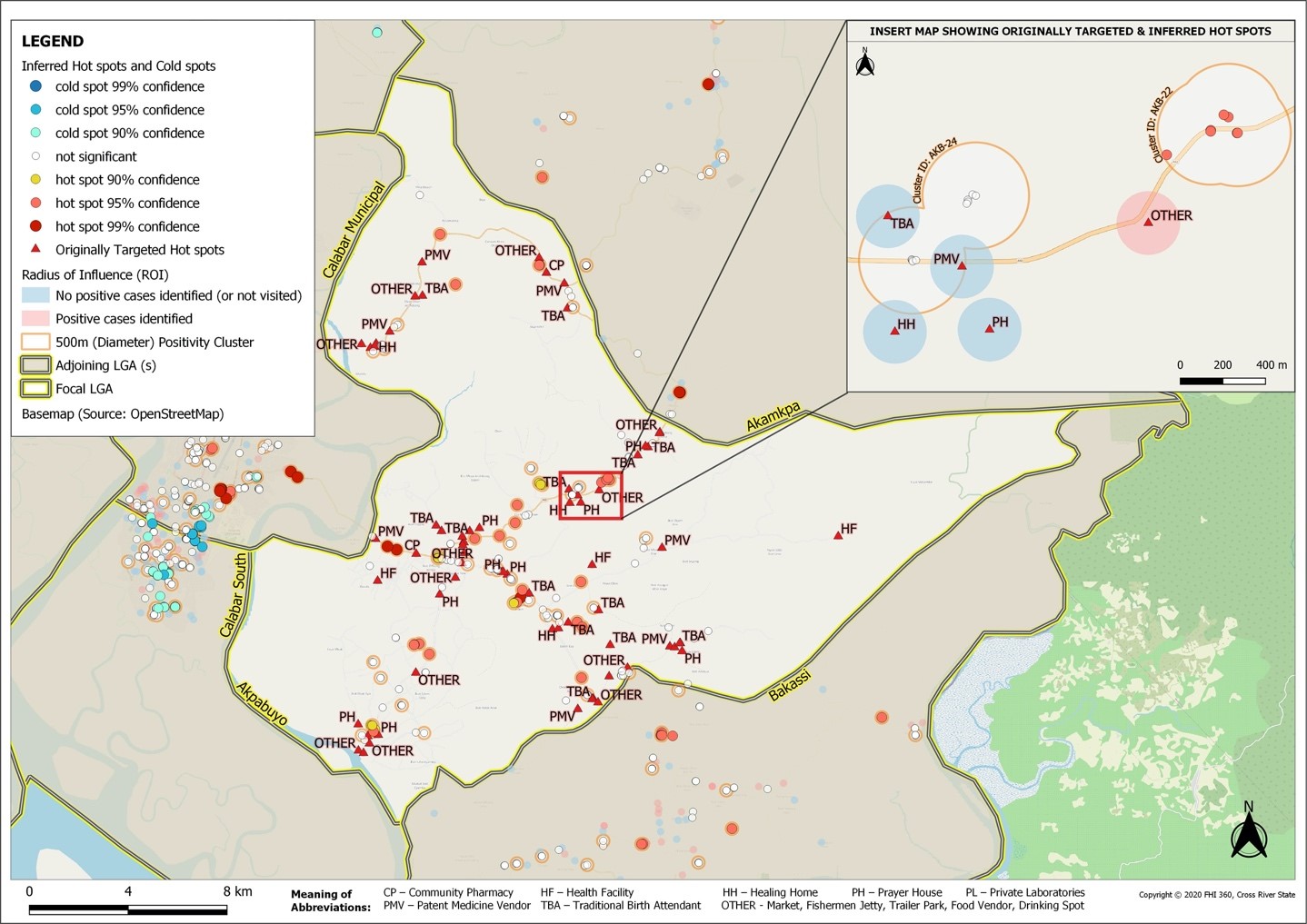
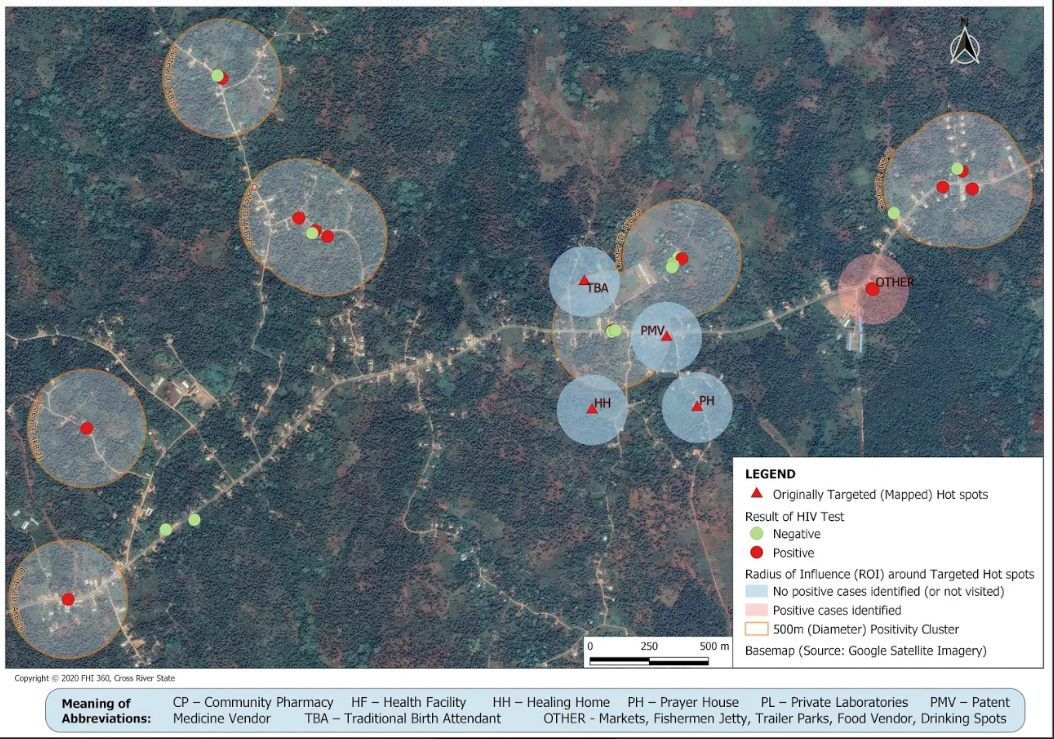
The second step was born out of the recognition of the possibility of using HIV testing data collected over time—which includes testing locations—to further map potential sites where the intended target population could be found. These testing locations were mapped (Figure 3) to show patterns in HIV positivity at a more granular (settlement) level to better streamline HIV testing to areas where previously undiagnosed cases are more likely to be located. This map identified 634 of these new potential locations, largely at the outskirts of urban centers and in the rural riverine communities with a large non-indigenous population of cross-border traders, fishermen, maritime workers, and inter-community taxi drivers. Possible transactional sex within and between this highly mobile population with a seasonal rural-urban migratory pattern could be responsible for the higher HIV positivity rates within these locations.
Figure 3. Detailed section of Akpabuyo LGA showing targeted hot spots, Cross River
Within nine weeks of implementing the GIS mapping from January to March 2020, 3,021 persons were offered HTS in the community including the hard-to-reach locations and residential areas along the creeks, and 703 individuals were found to be HIV positive and initiated on ART. This case-finding rate of 23.3 percent was much higher than the 8.0 percent at the facility (6,019 tested and 484 positives identified) during the same period.
In the nine weeks prior to implementing GIS mapping, only 53 cases were identified from testing 206 individuals in the community while at the facility during same period, 652 cases were identified from testing 8,518 (8 percent).
The GIS mapping gave the CAM teams guidance on what areas of the community to focus on and prioritize for HTS and case identification. This strategy therefore has the potential to accelerate the achievement of treatment saturation in Cross River.
