Bheki Sithole, Program Officer, EpiC Eswatini
Philisiwe Dlamini, Technical Officer, EpiC Eswatini
Laura Muzart, Project Director, EpiC Eswatini
Natasha Mack, Editor, Research Utilization, FHI 360
Pre-exposure prophylaxis (PrEP) is effective for HIV prevention when used correctly and consistently. At the Linkages across the Continuum of HIV Services for Key Populations Affected by HIV (LINKAGES) Eswatini project, we introduced PrEP in our core programming among key and priority populations—men who have sex with men, female sex workers and their clients, and transgender individuals—in 2019.
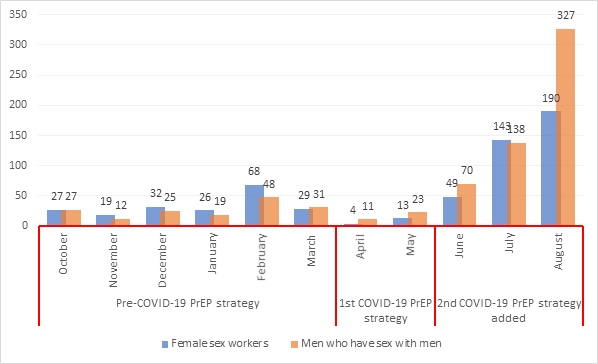
We have promoted PrEP on a nationwide scale, doing so at the community level through mobile clinic outreach within our standard comprehensive HIV and other health services. Nonetheless, PrEP has been slow to gain in popularity within the program. For instance, the average monthly initiation of PrEP from October 2019 to March 2020 under LINKAGES Eswatini was only 29 men who have sex with men and 37 female sex workers.
Due to the COVID-19 pandemic, programming shifted in April 2020 in order to take the necessary safety precautions for COVID-19 prevention, and the Ministry of Health suspended community-based HIV testing through August 2020. This meant that the mobile clinic outreach we had been using to provide PrEP and HIV treatment services was also required to cease operation.
We needed to develop alternative safe and innovative interventions to continue providing PrEP services, as well as increase uptake and continuation, during COVID-19. To come up with some new strategies toward this end, LINKAGES collaborated with key-population-led community-based organizations (CBOs) House of Our Pride, Health Plus for Men, Voice of Our Voices, and Rock of Hope.
The first strategy the group came up with was to mobilize the CBO and LINKAGES outreach workers, who were both members of key populations and HIV service users, to assess individuals for risk virtually, online, and by phone. Risk was assessed according to considerations of age, time since last HIV test, presence of sexually transmitted infections in the last six months, and condom use. People the outreach workers assessed virtually as being at high risk were offered an HIV self-testing kit, which they could pick up at any of more than 200 pickup points. Risk assessments were also conducted in person by the outreach workers manning the testing kit pickup points. Virtual assistance was then available once the individual was back home and ready to use the HIV self-testing kit. Those who screened HIV negative through the self-test and whose risk level was high were offered PrEP, which they could access at two key population drop-in centers in the two main towns in Eswatini, Mbabane and Manzini, which were still offering HIV services on certain days of the week.
However, despite these efforts, the transportation restrictions in place limited people’s ability to travel to the pickup points for the HIV self-testing kits being used for PrEP eligibility screening, as well as to the drop-in centers where PrEP could be accessed. As a result, PrEP initiations dropped to a monthly average of nine female sex workers and 17 men who have sex with men during April and May. So, we went back to the drawing board to see what strategies we could add that might make the difference.
The second strategy to encourage PrEP initiation which LINKAGES and our partners put into action emphasized convenience. This strategy, when added to the first, was able to boast more impressive results.
For the second strategy, from June through September 2020, we instituted mobile outreach focusing specifically on PrEP. First, peer outreach workers conducted HIV risk screening in small groups of no more than 10 people, or individually at people’s homes. This was done in areas close to where the outreach workers lived to accommodate the travel restrictions in place. People assessed to be at high risk were given two options: (1) they could use an HIV self-test right then and there and, if negative, be offered PrEP through PrEP-focused mobile outreach typically organized on a different day, or (2) based on their risk assessment results, they could be referred to the PrEP-focused mobile outreach for both the HIV testing and PrEP initiation, if eligible. Although community-based HIV testing had been stopped due to COVID-19, the government permitted mobile HIV testing in this context because it was a prerequisite to PrEP initiation. Individuals who tested positive were referred to HIV treatment and care services.
We also introduced what we called “PrEP ambassadors,” who were members of key populations and PrEP users themselves. Their task was to mobilize others within and beyond their networks for PrEP uptake by providing robust information on PrEP and ensuring linkages to HIV prevention services, including PrEP, at health facilities or drop-in centers established by LINKAGES and the key-population-led CBOs. Due to COVID-19, these PrEP ambassadors relied mostly on virtual mobilization (including social media, WhatsApp, and telephone calls), but also had limited one-on-one contact with some clients while taking COVID-19 precautions (i.e., wearing masks, social distancing, and applying hand sanitizer). The result was an increase in average monthly PrEP initiations to 115 female sex workers and 195 men who have sex with men (Figure 1).
LINKAGES also supported PrEP continuation by providing access to PrEP refills at two key population community centers, which we advertised to key populations on social media platforms (Figure 2). Pre-COVID-19, PrEP refills were obtained at clients’ facilities of choice, but once the pandemic hit, this access was affected by travel restrictions, people’s reluctance to seek out services at facilities, and the cessation of some services at the community level. The provision of PrEP refills in the two community centers ensured that PrEP users could continue to access their PrEP drugs easily.
In response to COVID-19, peer outreach workers and PrEP ambassadors provided more targeted PrEP outreach closer to the homes of key population individuals, whereas previously, outreach teams had divided their attention to provide diverse services. Anecdotal evidence indicates that the use of smaller outreach teams focusing specifically on PrEP services and catering to convenience has encouraged increased uptake and continuation of PrEP.

