Chris Akolo, Technical Director, HIV Department and EpiC, FHI 360
Caterina Casalini, Senior Technical Advisor Clinical Services, HIV Department, FHI 360
Danielle Darrow de Mora, Senior Technical Advisor, EpiC, FHI 360
Background
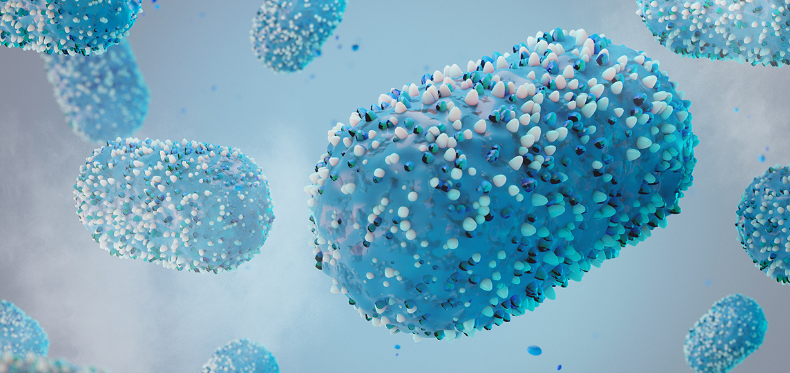
While the world was still battling the COVID-19 pandemic, another global epidemic, mpox, emerged. Mpox is an illness caused by a virus that passes from person-to-person through close contact. Endemic to Central and West Africa for decades, mpox is classified into two distinct clades: Clade I, previously known as the Congo Basin/Central African clade; and Clade II, the former West African clade.
In May 2022, an outbreak of Clade II mpox linked to sexual transmission and disproportionately affecting men who have sex with men (MSM) spread rapidly across Europe, throughout the Americas, and eventually to 114 countries. Soon after, in July 2022, the World Health Organization (WHO) declared mpox to be a public health emergency of international concern (PHEIC).
While less infectious and less virulent than COVID-19, the mpox outbreak suggested a growing trend of global health threats requiring readiness and a rapid, coordinated response. As Dr. Timothy Mastro, FHI 360’s Senior Science Advisor, said “Following the COVID-19 pandemic, the mpox epidemic serves as a further alarm for the need to improve our systems for public health response and ensure rapid access to diagnostic tests, vaccines and treatments.”
Global response
WHO led the global mpox response, collaborating with country- and regional-level health authorities, technical organizations, and financial institutions. It issued guidance about surveillance; readiness and response actions to strengthen laboratory systems; clinical care; infection prevention and control; and risk communication and community engagement (RCCE).
In May 2023, WHO declared an end to the PHEIC for mpox, as cases reported weekly declined from a global peak of 31,075 cases in August 2022, to an average of 712 cases globally each month from April through September 2023. However, on November 25, 2023, WHO published an mpox update outlining the virus’ ongoing and evolving epidemiology in the Democratic Republic of the Congo, where 12,569 suspected cases and 581 deaths were reported in 156 health zones in 22 out of 26 (85%) provinces since January 2023. Newly identified outbreaks related to the sexual transmission of Clade I mpox were also reported.
Most of these cases were identified through sexual health or other health services in primary or secondary health care facilities, with most reported cases with known data on sexual behavior (83.2%) occurring among MSM. Both the May 2022 and May 2023 outbreaks were driven by sexual transmission that primarily affected MSM.
Mpox and HIV
Mpox disproportionately affects people living with HIV (PLHIV), who have accounted for up to half of diagnoses globally. Similar to HIV-associated opportunistic infections, mpox produces substantially greater morbidity and prolonged disease in people with advanced or untreated HIV infection. The emergence of mpox as an opportunistic infection highlights the need for continued aggressive, comprehensive strategies for HIV testing, prevention, linkage to care, and treatment services to prevent HIV infection or disease progression that will reduce risk for severe mpox and mitigate its impact. Along with providing access to mpox vaccination and to services for sexual health and prevention for those who are at risk for mpox and HIV, these actions can diminish the potential of mpox to present as an HIV-associated opportunistic infection.
EpiC’s global response to mpox
The Meeting Targets and Maintaining Epidemic Control (EpiC) project, funded by U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and the U.S. Agency for International Development, has been involved in the global response to mpox since June 2022. EpiC’s global footprint, along with its ability to provide technical assistance, allowed for rapid response with effective tools, capacity building, and monitoring and evaluation. In August 2022, the project began offering technical assistance to partner governments to accelerate the emergency response to mpox. This response focused on three main areas:
- Supporting surveillance and laboratory capacity. To detect and confirm mpox cases and monitor the spread of the virus, EpiC provided technical assistance, training, and equipment to national and regional laboratories in Africa, Asia, Europe, and Latin America, and supported the development and validation of new diagnostic tests for mpox.
- Strengthening infection prevention and control (IPC). To reduce the risk of transmission and exposure to mpox among health workers and communities, EpiC helped implement IPC measures in health facilities and community settings by providing personal protective equipment, disinfectants, and waste management supplies, and conducted IPC assessments, audits, and trainings for service providers, including those at the community level.
- Enhancing social and behavioral change (SBC) messaging. To raise awareness and promote preventive behaviors among populations at risk of acquiring mpox, EpiC designed and delivered evidence-based SBC interventions. This included mass media campaigns, community dialogues, peer education, and mobile phone messages to inform people about the symptoms of mpox, its transmission modes, prevention methods, and available treatment options. EpiC also adapted the multi-country online app QuickRes that uses online reservation and case management software for enhanced communication and reporting on mpox.
Examples of FHI 360’s work in action:
- Through the EpiC project, FHI 360 and its partners worked in Benin, Ghana, Morocco, the Dominican Republic, Jamaica, and Guatemala to respond and bolster the response to mpox by supporting countries and communities at higher risk of acquiring mpox in RCCE activities, providing training and capacity building for health care providers, and supporting community-based surveillance and contact tracing.
- EpiC’s response to mpox has been coordinated with WHO, national governments, other international organizations, and local partners. EpiC also contributed to the global health agenda by sharing its experience and lessons learned from the mpox outbreak response with other stakeholders by participating in relevant forums and events.
Looking forward
Newly emerging and re-emerging viral infections represent a significant public health concern today. If we fail to act swiftly and effectively against mpox, the virus will spread further and reach new animal reservoirs. An mpox outbreak could become endemic outside Africa, posing a constant threat of re-emergence and mutation. It even has the potential to evolve and become more transmissible, virulent, or resistant to existing vaccines or drugs.
Key considerations going forward:
- Like COVID-19, the mpox outbreaks provided an opportunity for better surveillance, early detection, and response capacities for emerging infectious diseases, especially those that can cross borders and species. More and better surveillance, health care provider training, and community monitoring will continue to be critical.
- The outbreak prompted increased cooperation and coordination among countries and stakeholders. It also underscored that to effectively prevent, prepare, and respond to future mpox outbreaks, continuous collaboration and coordination among scientists, policymakers, health care professionals, and the public is required.
- Analysis of mpox data is continuing to better understand presenting conditions, morbidity and mortality, and subgroup analysis in key populations with the aim of helping clinicians and national programs optimize patient management and public health response strategies. Prospective global studies of antivirals for this disease, as well as vaccines to eliminate mpox are needed. In particular, more data on the efficacy and safety of mpox medications among PLHIV, as well as the potential interactions with antiretroviral therapy, will be critical.
- Prevention and control strategies should include addressing misinformation, stigma, and discrimination, particularly among PLHIV and key populations as mpox can disrupt their access to HIV services. WHO guidance provides information on the potential impact of stigma and recommends language and actions to counter stigmatizing attitudes and discriminatory behaviors and policies.
- There are many parallels in the inequity of COVID-19 and mpox vaccine and treatment availability for lower income regions such as Africa and Latin America, highlighting the need to prioritize and support local manufacturing capacity for vaccines in low- and middle- income countries.
In the long-term, a One Health approach is needed, acknowledging the interconnection and interdependence of the health of people, animals, plants, and the environment aims to achieve optimal health outcomes for all living beings. Focusing on systems strengthening, cross-sectoral collaboration, and integrating measures to mitigate the socio-economic effects of outbreaks could prepare us for future outbreaks of mpox and other new and re-emerging infectious diseases.
Featured image: Photo credit: LumerB/Getty Images
United States Agency for International Development (USAID) engaged the Meeting Targets and Maintaining Epidemic Control (EpiC) project as an mpox technical assistance provider, leveraging EpiC’s global footprint and ability to support surveillance and laboratory capacity, strengthening infection prevention and control, and enhancing social and behavioral change messaging. EpiC provided technical assistance to partner governments in six countries to accelerate the emergency response to mpox. Read more about EpiC’s mpox work and access technical resources here.