Gift Kambandanga, Project Manager, EpiC, PSI Malawi
Philip C. Mkandawire, Market Development, Social Franchise & Research, Deputy Chief of Party, PSI Malawi
Lirica Nishimoto, Technical Officer, EpiC, FHI 360
Moses Bateganya, Technical Director, EpiC, FHI 360
With more than 850,000 people living with HIV (PLHIV) on antiretroviral therapy (ART) in Malawi, the public health system is under enormous strain to meet treatment initiation and retention needs of these clients. Solutions are needed to reduce this burden on the system while making it easier for clients to access high quality treatment services. The COVID-19 pandemic has made the need to decongest public health facilities even more pronounced to decrease risk of COVID-19 transmission to clients as well as to health facility staff.
The private medical sector in Malawi is small but growing and could be leveraged to improve treatment access and retention for PLHIV. Private clinics are well equipped to provide standard HIV services and are often closer to where PLHIV live and work than government health facilities. Dispensing antiretrovirals (ARVs) through private clinics has the potential to reduce barriers to treatment access for PLHIV and decongest public facilities. To explore this potential, the Meeting Targets and Maintaining Epidemic Control (EpiC) project piloted a decentralized ARV drug distribution (DDD) model, in which PLHIV established on treatment and receiving ARVs through public health facilities were devolved to private clinics for refills and ongoing care. The pilot was implemented in four districts: Mulanje, Machinga, Kasungu, and Mangochi.
Laying the groundwork
The private sector DDD model was approved by Malawi’s Ministry of Health (MOH) in September 2020. Prior to rollout, the EpiC Malawi team — led by FHI 360 and PSI — laid the groundwork for implementation.
The EpiC team first conducted interviews with 82 ART clients and 17 ART coordinators from 17 public health facilities to assess their interest in the DDD model. Of clients, 72% were interested in the model (Figure 1); 57% were willing and 22% were somewhat willing to pay a fee for the service. Among those willing and somewhat willing, the most commonly reported acceptable service fee was MK500 (~US$0.62). The interviews also identified factors that ART clients felt were most important for ARV pickup locations, which included convenience, privacy, and proximity to where clients live.
ART coordinators reported that the model would reduce the workload at public facilities, provide an opportunity to clients on ART to have flexible refill times, and facilitate improved service quality since providers would have more time to spend with clients who need more intensive care, such as those newly initiated on ART and those with advanced HIV disease.
Following this assessment, a team of representatives from the MOH, Malawi Business Coalition against AIDS (MBCA), Medical Council of Malawi (MCM), and Pharmacy Medicines Regulatory Authority (PMRA) accredited 10 private clinics to pilot the DDD model based on the following criteria: availability of the adequate number of clinical or nursing staff, willingness of clinic staff to participate in DDD, clinic staff trained on ART, appropriateness and readiness of infrastructure, appropriateness of both internal and external security, and compliance with MCM and PMRA requirements. The clinic providers were then trained to implement the model, including to manage clients starting or continuing ART according to national standards. A service fee of MK1000 (~US$1.23) was agreed upon between the clinics and MBCA.
Raising awareness and reducing client burden
Findings from the interviews were used to inform the development of promotional materials and messages to raise awareness and generate interest in the DDD model among ART clients. Key messages included:
- Don’t be hard on yourself ‘osamaukhwimitsa moyo’ — now you can access ART services from private clinics in your area.
- Be in charge of the time and day to get your ART refills.
- Accessing ART at the private clinic is safe and discreet.
- Save time, get your refill at your nearest private clinic.
- A viable option that works for you; now you can get your ART refills at your nearest private clinic.
- Beat the queue, refill at your nearest private clinic.
Expert clients (ECs) are PLHIV established on treatment who have a good understanding of HIV care and treatment services and help other PLHIV access and navigate HIV services. They, as well as PLHIV support groups, were identified as ideal for providing DDD information. A one-day training was held with 42 ECs to strengthen their knowledge about DDD and how to encourage peers to enroll.
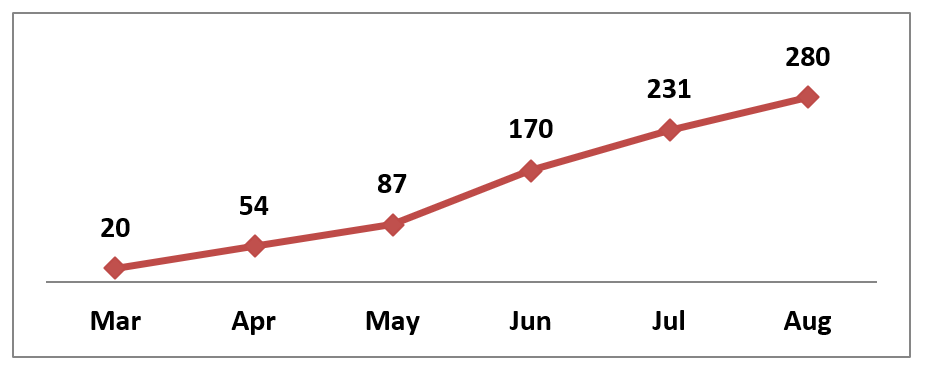
DDD implementation, including demand generation activities with ECs, began in March 2021; however, initial uptake was slow. After discussions initiated by EpiC, the dispensation fee of MK1000 per one-month supply was reduced by MCBA to MK300 per visit, regardless of the number of months of ARVs dispensed. The reduced fee was communicated to PLHIV through ECs, and by the end of June 2021, enrollment started to increase. By August 2021, a total of 280 clients from 13 public health facilities had picked up ARVs from one of the 10 private clinics participating in the pilot (Figure 2). Enrolled clients have expressed excitement about this new model.
“This is timely with COVID-19 as there are no congestions here.”
“Wish the model started sometime back; it’s a game changer.”
“No long queues. We are treated as kings and queens.”
Though small, this initial achievement is encouraging. The project continues to make progress by maximizing community awareness of DDD through community radio, television stations, and targeted community meetings to retain more clients on ART and contribute positively to the 95-95-95 UNAIDS targets. Integrating private clinics into their routine ARV supply chain, the MOH is already showing interest in sustaining the model. DDD through private clinics in Malawi holds promise for increasing access to ARVs and improving continuity of treatment for PLHIV both during and beyond COVID-19.
Photo Credit: EpiC Malawi