Lirica Nishimoto, Technical Officer, EpiC
Michael Odo, Technical Advisor, EpiC Liberia
Moses Bateganya, Director, Technical, EpiC
Danielle Darrow de Mora, Technical Advisor, EpiC
Julia Toomey, Project Manager, National AIDS Control Program
Liberia has an estimated 40,000 people living with HIV, 46 percent of whom are on life-saving antiretroviral therapy (ART). About 70 percent of those on ART reside in the country’s capital, Monrovia, and most access ART from just a few health facilities. With only six health care workers (doctors, nurses, or midwives) per 10,000 population—well short of the critical threshold of 23 per 10,000 recommended by the World Health Organization—Liberian health facilities are typically congested, putting significant pressure on a fragile health system weakened by 14 years of civil war, the deadly Ebola epidemic, and now the COVID-19 pandemic. This context, coupled with pervasive stigma toward people living with HIV and key population members, contributes to suboptimal clinical outcomes, including high rates of treatment interruption.
Addressing barriers to ART
To better understand barriers to ART access among people living with HIV in Liberia, the Meeting Targets and Maintaining Epidemic Control (EpiC) project funded by the United States Agency for International Development (USAID) and the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) collaborated with the National AIDS Control Program (NACP) to conduct an assessment with 58 ART clients as key informants in Monrovia. The top challenges identified were long wait times at the health facility and cost of transportation (Figure 1). Among respondents, 93 percent reported waiting more than an hour on average for services at the health facility, and nearly 60 percent reported traveling an hour or more to their ART pickup location. However, among the 43 respondents (74 percent) who had used private pharmacies in the past, nearly 80 percent reported a travel time of less than 30 minutes to reach a pharmacy.
In light of these findings, the EpiC Liberia team and NACP agreed to introduce decentralized drug distribution (DDD) as a way to ease the burden on ART clinics and address some of the barriers that people living with HIV face in accessing treatment. DDD—the delivery of ART outside of health facilities, including via the private sector and at alternative pickup points—is a modality of differentiated service delivery (DSD) that can make ART services more convenient and client-centered. DDD is included in Liberian health policy, which promotes ART dispensing to recipients in the ‘right manner, at the right place and for the right persons’ to optimize the benefits of treatment.
Pharmacies selected and prepared for implementation
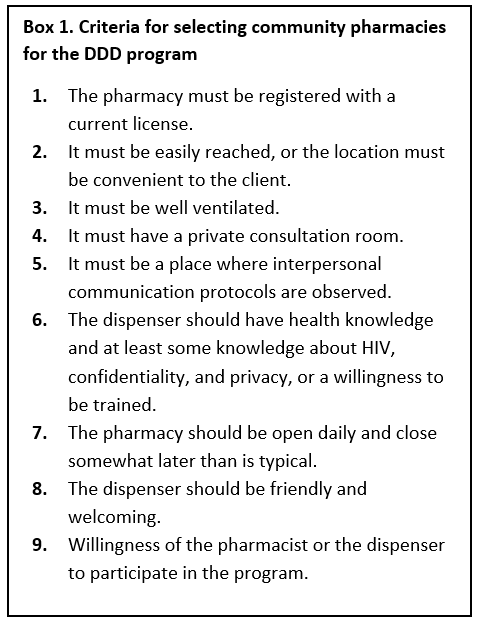
In October 2020, NACP selected Redemption Hospital, an intra-urban high-volume ART clinic that sees an average of 80 people living with HIV daily, to pilot DDD of ART through community pharmacies (CPs). This model devolves stable ART clients from public facilities to pick up their drugs at a CP of their choice and return to the health facility only for a clinical review and viral load (VL) test or if they have a medical condition. With technical assistance from EpiC, a joint team made up of NACP, the Liberia Pharmacy Board, and the Liberia Network of People living with HIV (LibNeP+) assessed 198 CPs in Montserrado to understand their readiness and willingness to dispense ART using standardized tools. Of those assessed, the majority (97 percent) were willing to dispense ART, and 75 percent were open in the evenings and on weekends. Many were in suburbs with a high population density. Forty-one CPs met the criteria set by the team for DDD participation (Box 1), and 15 CPs located in suburbs where most ART clients lived were selected for initial rollout. Some pharmacies declined to participate for fear of being associated with people living with HIV, an indication of the high level of stigma toward this population in Liberia.
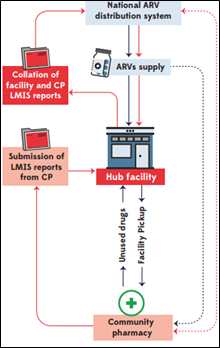
Together with the facility ART team, pharmacists and other staff from selected CPs were trained on basics of HIV and ART management, including the processes for dispensing ART in the community, ensuring uninterrupted supply chain, sending clients reminders related to adherence, making referrals, and managing data (Figure 2). A referral directory and the DDD electronic application (DDD App) were adapted to provide a seamless interface for information on devolved clients between hub facilities and CPs. The DDD App allows for easy communication between the health facility and pharmacies to ensure fast data exchange and can be configured to send text reminders to clients. The parties signed a memorandum of understanding that stipulates the roles and responsibilities of the partners, who consist of the government (represented by NACP), the regulatory body (pharmacy board), participating CPs, and the health facilities.
Looking ahead
In the first five weeks of implementation, the hospital successfully transferred 37 people living with HIV to 13 CPs for their next refill. Both the health care workers and LibNeP+ have expressed satisfaction at the prospect of ART clients receiving their ARVs within walking distance of their homes. This early success of the CP model holds promise and will continue to be implemented in Liberia with close monitoring of its impact on client ART access and retention.